A Chinese proverb aptly compares wealth to the number zero (0), with increased accumulation corresponding to a greater number of zeros. Health, conversely, is symbolized by the number one (1) preceding these zeros. This adage underscores the notion that wealth (the zeros) without good health (the preceding one) is ultimately valueless, rendering good health the most invaluable asset. Given the widespread prevalence of various diseases, acquiring knowledge about these ailments is of paramount importance. Diseases can be broadly categorized into two groups: infectious diseases (ID) and noncommunicable diseases (NCD).

In conjunction with NCDs, infectious diseases caused by pathogens account for millions of fatalities annually. The etiology of infectious diseases is multifaceted, determined by factors such as pathogen classification and an individual’s immune system strength.
In healthy individuals, pathogens may not necessarily incite immediate disease. However, when the immune system is weakened, these pathogens can swiftly become perilous. The course of an infection is contingent upon the body’s response to the invading pathogens.

Infectious diseases (ID) are subdivided into two categories:
- Communicable Infectious Diseases (CIDs): CIDs encompass diseases instigated by bacteria, viruses, or pathogens that can be transmitted among humans, including influenza, tuberculosis, encephalitis, and polio.
- Non-Communicable Infectious Diseases (NIDs): NIDs comprise infectious diseases elicited by bacteria, viruses, or pathogens that cannot be transmitted to others, such as cystitis, necrotizing fasciitis, gangrene, and nephritis.
Pathogens: The Origins of Human Maladies
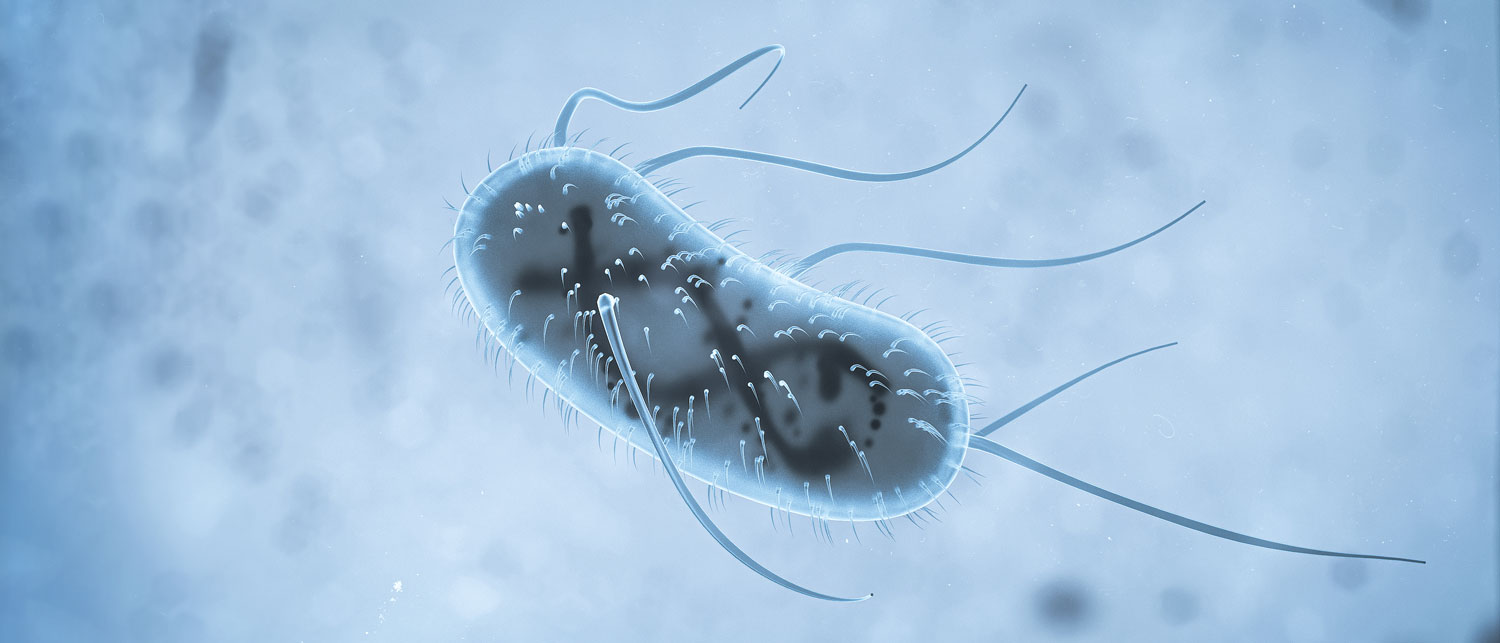
Infectious agents are microorganisms that proliferate and reproduce within the bodies of other organisms. These microorganisms can invade and inhabit the bodies of other animals or “hosts,” resulting in infection and potentially fatal diseases.
Viruses are microscopic microorganisms composed of genetic material (nucleic acids), a protein coat (capsid), and a lipid envelope. Their genetic material may be either RNA or DNA. Viruses necessitate host cells from other organisms for survival and replication. Viral infections can modify host cells, causing cell death, altered cell properties, or malignancy.
Treatment: Vaccines and antiviral medications. Some viral infections pose treatment challenges.
Examples: Influenza, Coronavirus Disease-2019 (COVID-19)
Bacteria are simple, single-celled organisms consisting of proteins and carbohydrates. They are omnipresent in the environment. Bacterial infections can infiltrate host cells through wounds, ingestion, inhalation, or, in some instances, compromised immune systems. Resident bacteria within the host’s body can also induce diseases and illnesses..
Treatment: Antibiotics and adherence to good personal hygiene.
Examples: Cholera, Tuberculosis, Tetanus

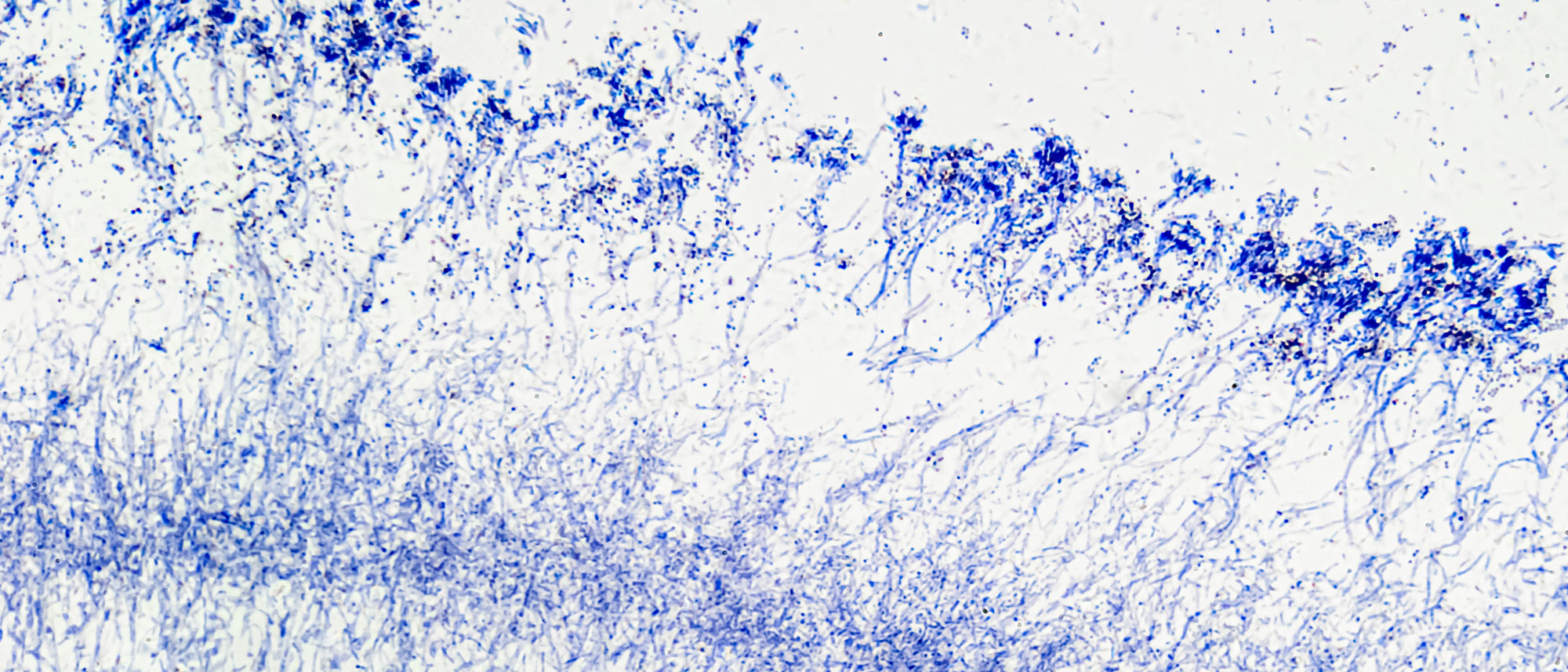
Fungi, encompassing yeasts and molds, are multicellular organisms that exhibit diverse sizes and shapes. Fungi reproduce asexually via division and spore dispersal into the air. Most fungal infections arise from direct spore contact or inhalation, leading to skin and respiratory diseases. However, fungal infections are relatively uncommon in individuals with robust immune systems.
Treatment: Topical or oral medications. Preventively, avoiding direct contact with harmful fungi is strongly advised.
Examples: Athlete’s foot, eczema, and tinea
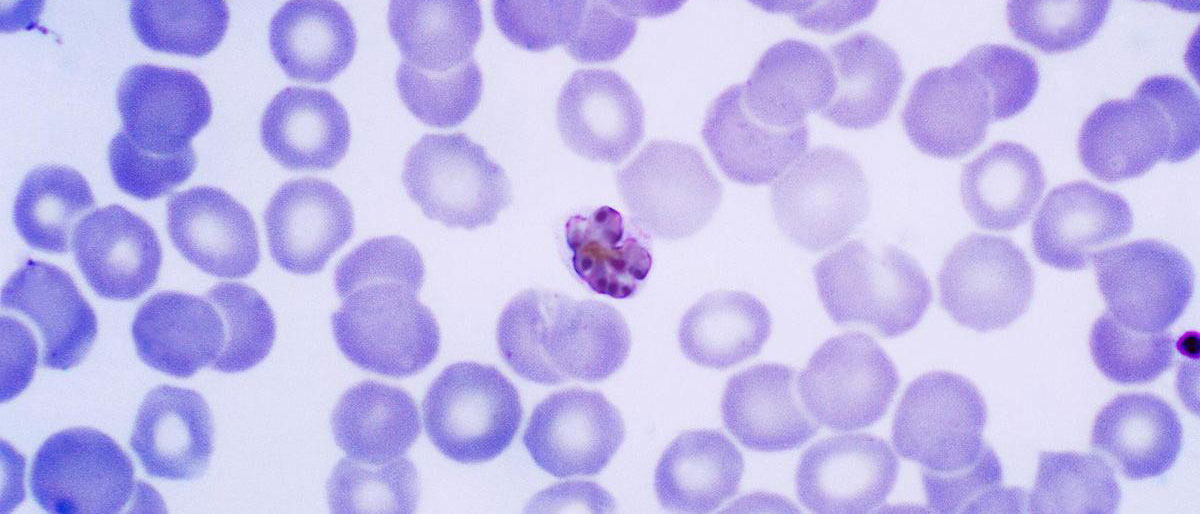
Protozoa are single-celled organisms exhibiting animal-like traits. They can reproduce multiple times throughout their lifespan and propagate through various means, including host changes, food and water contamination, or insect transmission as carriers to reproduce and locate new hosts. Protozoan infections can infiltrate the host’s body through the digestive and circulatory systems, among other pathways, employing mechanisms akin to viruses.
Treatment: Antiprotozoal drugs and adherence to good personal hygiene. As a precautionary measure, avoiding direct contact with protozoan sources is recommended.
Examples: Malaria caused by the protozoan “Plasmodium” transmitted by mosquitoes
Parasites are the largest multicellular organisms among the five infectious agents. They can be observed with the naked eye and inhabit saltwater, freshwater, and moist environments. At various developmental stages (egg, larva, or adult), some parasites can directly penetrate the host’s skin or enter host cells via the lymphatic or circulatory systems, ultimately reaching vital organs such as the heart and lungs, or invading the digestive system to mature into adults within the small intestine, siphoning nutrients from the host.
Treatment: Antiparasitic drugs and maintaining good personal hygiene. As a precautionary measure, avoiding direct contact with parasite sources is highly recommended.
Examples: Hookworm infection, Ascariasis
In 2020, the Coronavirus (CoV) evolved into the most severe and pervasive viral outbreak worldwide. The World Health Organization (WHO) officially elevated the status of COVID-19 from an epidemic to a global pandemic. This designation applies to newly emerging infectious diseases that spread on a global scale, leading to a significant rise in morbidity and mortality rates.
COVID-19, a novel strain of coronavirus, surfaced and disseminated globally. The scale of infections and fatalities escalated worldwide, with the virus mutating into new strains during the development of potential vaccines.
Statistical data is indicative of the severity and breadth of COVID-19’s impact. The virus is transmitted through respiratory droplets, spread by coughing, sneezing, saliva, and nasal discharge. The virus can persist for several days on uncleaned surfaces or objects. Direct contact with these contaminated surfaces or close physical contact with an infected individual can facilitate the spread of the virus.
The COVID-19 pandemic has a global reach, but it is not the first pandemic to occur. Since the turn of the century, multiple pandemics have surfaced. Each one is characterized by a unique set of causes, transmission methods, and levels of severity:
- Severe Acute Respiratory Syndrome (SARS-CoV-1) has a mortality rate of 10%.
- Middle East Respiratory Syndrome (MERS-CoV) has a mortality rate ranging between 30 and 40%.
- Ebola has an approximate mortality rate of 50%.
- Seasonal influenza, caused by various influenza viruses, has a mortality rate of 0.1%.
- COVID-19, or Coronavirus Disease (SARS-CoV-2), has a mortality rate of 3%.

Based on the above, it is evident that pandemics are becoming more frequent. The most alarming of these are viral pandemics, as there are no vaccines that can wholly prevent or treat viral diseases. The ability of viruses to mutate adds an additional layer of complexity and time to vaccine development.
Despite having a lower mortality rate than SARS, MERS, or Ebola, which have mortality rates between 10% and 50%, the ongoing COVID-19 pandemic is a cause for grave concern. The incubation period of COVID-19, extending up to 14 days, is longer than that of many other infectious diseases, during which time individuals may be asymptomatic. This can result in the unwitting creation of asymptomatic carriers of COVID-19, leading to widespread transmission. This factor sets COVID-19 apart from other diseases, where the rapid onset of symptoms limits opportunities for disease transmission. Additionally, unlike other diseases, COVID-19 is not confined to a specific outbreak area. Furthermore, the novel coronavirus, similar to SARS-CoV-1, binds to respiratory mucosa cells via the ACE2 receptor more effectively, escalating the severity of the disease. The virus targets protein enzyme ACE 2 receptors to infiltrate cells, multiply within lung cells, and continue to infect neighboring cells, thereby accelerating its spread.
Infectious agents, such as viruses and bacteria, are often invisible to the naked eye, posing a constant risk of exposure. The fact that we only fall ill occasionally or infrequently is testament to the effectiveness of our immune system. Fortunately, humans possess a primary immune mechanism known as the Innate Immune System (IIS), which serves as our first line of defense against invading pathogens.
While this immune response is not specialized to a particular pathogen, it often falls short in defending against contemporary viruses due to their constant mutation. The reasons behind these viral mutations depend on factors that influence the growth of the virus, and these can be classified into three categories:
- Geographic factors, such as regions or nations prone to frequent outbreaks.
- Climatic conditions, which have been shown to influence the development of viruses like the coronavirus when outside the human body. For instance, the tropical climate of countries like Thailand is considered unfavorable for the growth of the coronavirus.
- Environmental factors, with viruses finding it easier to spread in overcrowded conditions, thus increasing the risk.
Should a pathogen successfully breach the Innate Immune System (IIS), the body activates the Adaptive Immune System (AIS) in response to exposure to unfamiliar pathogens or viruses. The AIS will combat these pathogens, though it requires time to adapt and respond effectively to assaults from harmful pathogens before ultimately eliminating them. The duration for the AIS to mount a response varies based on individual physiological characteristics.
Based on the above, it is evident that pandemics are becoming more frequent. The most alarming of these are viral pandemics, as there are no vaccines that can wholly prevent or treat viral diseases. The ability of viruses to mutate adds an additional layer of complexity and time to vaccine development.
Despite having a lower mortality rate than SARS, MERS, or Ebola, which have mortality rates between 10% and 50%, the ongoing COVID-19 pandemic is a cause for grave concern. The incubation period of COVID-19, extending up to 14 days, is longer than that of many other infectious diseases, during which time individuals may be asymptomatic. This can result in the unwitting creation of asymptomatic carriers of COVID-19, leading to widespread transmission. This factor sets COVID-19 apart from other diseases, where the rapid onset of symptoms limits opportunities for disease transmission. Additionally, unlike other diseases, COVID-19 is not confined to a specific outbreak area. Furthermore, the novel coronavirus, similar to SARS-CoV-1, binds to respiratory mucosa cells via the ACE2 receptor more effectively, escalating the severity of the disease. The virus targets protein enzyme ACE 2 receptors to infiltrate cells, multiply within lung cells, and continue to infect neighboring cells, thereby accelerating its spread.
Durascience™ has pioneered the development of P.P.M™, a cutting-edge strategy designed to fortify the immune system’s ability to defend against infectious agents. The Durascience™ Institute in the U.S.A. concentrates on the scientific principle of P.P.M™ (Pathogen Prevention Matrix), striving to enhance immune system function and improve quality of life across all ages (Eternity of all ages).
The immune system plays a pivotal role in determining the severity of infections resulting from pathogen invasion. It is well-established that immune system efficacy fluctuates with age due to variations in lifestyle, environment, and personal health conditions. As the immune system is in constant flux, maintaining its vigor is crucial to ensure that the body is equipped to combat harmful pathogens. The following are straightforward yet effective strategies for bolstering immune function:
- Consume recommended servings from each of the five food groups.
- Engage in regular physical activity.
- Ensure adequate sleep.
- Obtain essential nutrients, such as protein and zinc.
- Receive age-appropriate vaccinations.
By adhering to a healthy environment and avoiding high-risk viral transmission areas, the immune system can be further fortified. Implementing these recommendations will help ensure robust immune defense, empowering individuals to lead healthy lives with confidence.
Based on the above, it is evident that pandemics are becoming more frequent. The most alarming of these are viral pandemics, as there are no vaccines that can wholly prevent or treat viral diseases. The ability of viruses to mutate adds an additional layer of complexity and time to vaccine development.
Despite having a lower mortality rate than SARS, MERS, or Ebola, which have mortality rates between 10% and 50%, the ongoing COVID-19 pandemic is a cause for grave concern. The incubation period of COVID-19, extending up to 14 days, is longer than that of many other infectious diseases, during which time individuals may be asymptomatic. This can result in the unwitting creation of asymptomatic carriers of COVID-19, leading to widespread transmission. This factor sets COVID-19 apart from other diseases, where the rapid onset of symptoms limits opportunities for disease transmission. Additionally, unlike other diseases, COVID-19 is not confined to a specific outbreak area. Furthermore, the novel coronavirus, similar to SARS-CoV-1, binds to respiratory mucosa cells via the ACE2 receptor more effectively, escalating the severity of the disease. The virus targets protein enzyme ACE 2 receptors to infiltrate cells, multiply within lung cells, and continue to infect neighboring cells, thereby accelerating its spread.


Genetics
Research from King’s College London indicates that approximately 75% of the immune system is genetically influenced. In a study involving 497 adult female twins, 23,000 immune system characteristics were analyzed, revealing that the adaptive immune system (AIS) was significantly impacted by genetic factors. The findings also suggest that genetic variations have a more considerable effect on the adaptive immune system than previously believed, while the innate immune system is more vulnerable to environmental influences.
The human body harbors a diverse array of microorganisms, including bacteria residing in the digestive tract, collectively known as the microbiome. The gut microbiome plays a vital role in health, influencing energy metabolism, hormone regulation, bone health, skin condition, and immune system function. Our digestive system houses trillions of bacteria from over 1,000 species, predominantly firmicutes and bacteroidetes. The gut microbiome’s balance is affected by factors such as diet, illness, antibiotic use, and aging.
Recent studies utilizing modern techniques have demonstrated that these microbes significantly impact various body systems, including the circadian rhythm, metabolism, and immune system. Microbes play a crucial role in immune system development during childhood, with the balance of microbes stabilizing in adulthood. The infancy stage may be the most critical period for immune system development.
Proper nutrition is paramount for maintaining a healthy immune system, as malnutrition is the leading cause of immune system impairment. Deficiencies in essential nutrients such as zinc, selenium, iron, copper, and vitamins A, C, E, and B6 can hinder immune system performance. Obesity can also negatively impact the immune system, as can macrosomia (a baby being overweight at birth). Consuming zinc-rich foods can help address these issues.
The immune systems of older individuals, who experience a gradual decline in immune system efficiency, can also benefit from consuming a diverse range of essential nutrients.

The accumulation of free radicals in the body can damage cell membranes, enzymes, and intracellular substances, ultimately disrupting and impairing the immune system. The immune system is particularly sensitive to free radical damage due to its reliance on cell contact mechanisms, such as receptors, which have membranes primarily composed of fatty acids. Free radicals can harm fatty acids in cell membranes.
A robust antioxidant system can help mitigate the damage caused by free radicals, allowing the cellular structures of the immune system to resist damage and remain strong. Implementing a balanced diet rich in antioxidants, such as vitamins C and E, beta-carotene, and selenium, can contribute to a more effective anti-inflammation system.
Recognizing the distinctions between the Innate Immune System and the Adaptive Immune System is crucial. The innate immune system is active from birth, immediately responding to pathogens by encapsulating and neutralizing them. This system also bolsters the adaptive immune system, which generates antibodies through B lymphocytes (or B cells).
While the adaptive immune system takes longer to react to new pathogens initially, it is more efficient at identifying recurring pathogens. Throughout life, factors such as pathogen exposure and vaccinations influence the adaptive immune system. Healthy genetic traits promote effective immune system functionality and immune cell sensitivity to pathogen infiltration. However, the efficiency of genes encoding vital immune system proteins declines with age.

The establishment of intestinal bacteria during infancy is influenced by factors such as breastfeeding and a nutrient-rich, balanced diet. A robust gut microbiome enhances both intestinal function and immune system performance. As individuals age, the immune system and microbial balance in the digestive system undergo changes, promoting immunization from the intestines to the bloodstream.
Extensive research has indicated that optimizing the digestive system’s balance positively affects immune system function, mitigates mild inflammation, and improves overall health and life expectancy.
Consuming adequate nutrition from early childhood prepares both immune systems for effective operation. Numerous studies have demonstrated that nutrient intake profoundly impacts immune system performance, particularly during the aging process. Over time, the absorption of various nutrients decreases, ultimately influencing the immune system. In older adults, alterations occur in the balance of T and B systems, immune system cell development, and overall immune cell function.

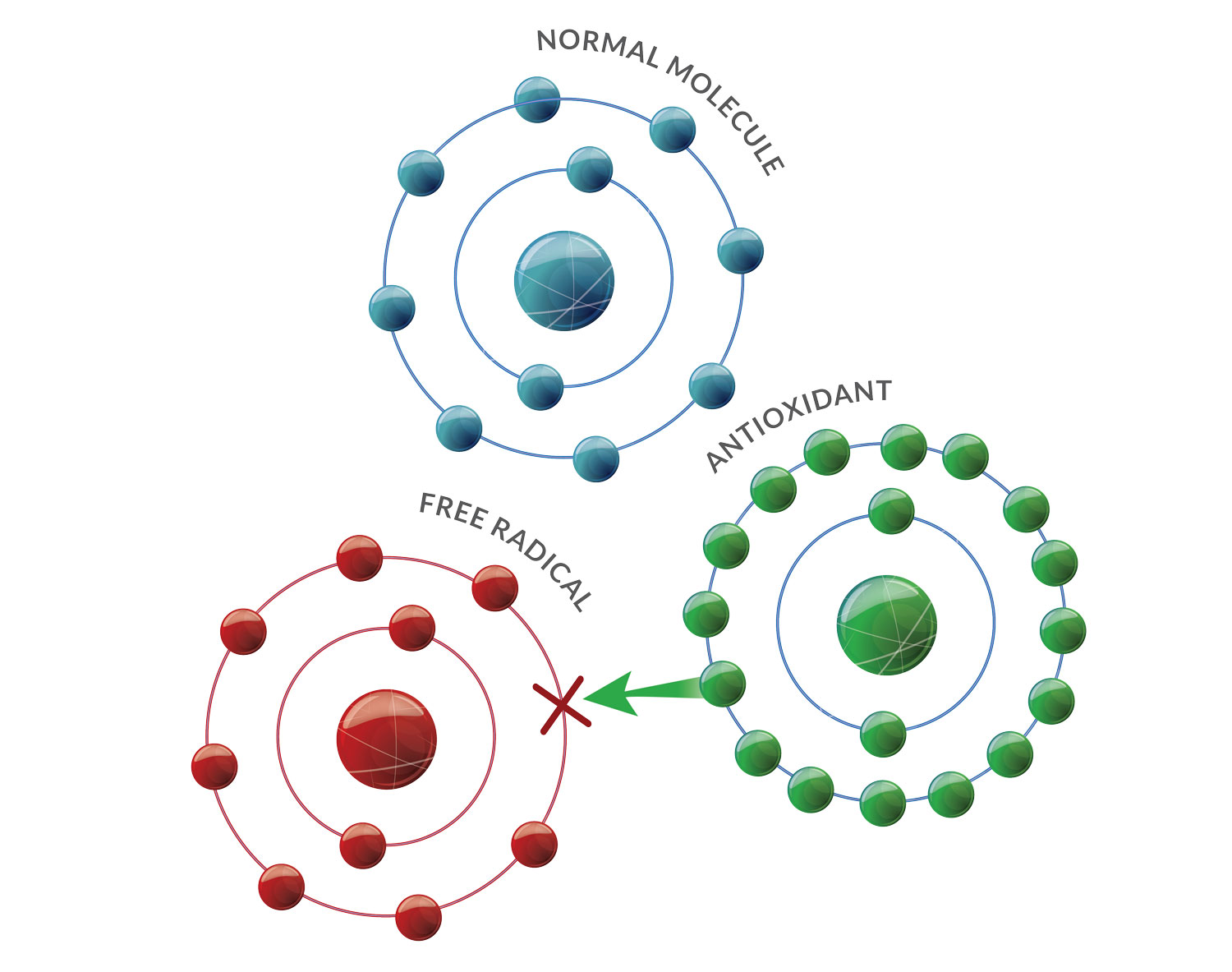
During childhood, the body encounters an array of free radicals that adversely affect cellular function. However, most children possess an efficient antioxidant production process, allowing cells within different systems to operate and grow normally, thereby ensuring a well-functioning immune system.
Free radicals, such as Reactive Oxygen Species (ROS) or Reactive Nitrogen Species (RNS), originate from both standard metabolic processes within the body and external sources like food and pollution. The accumulation of free radicals leads to oxidative stress, inflicting damage on proteins, fats, and DNA within cells. Consequently, this damage results in cellular degeneration and aberrant immune system functioning.
The Consequences of P.P.M™ Component Deficiency
Genetics are instrumental in the growth and development of the immune system from birth, exerting a direct influence on immune function and response. Primary immunodeficiency disorders can manifest from birth, inherited across generations. Symptoms may encompass early mortality, delayed development, or persistent and severe infections during childhood.

In adults and the elderly, the gene-regulated cell production in the immune system at the bone marrow and thymus gland also experiences a decline. This reduction directly impacts the number and efficacy of immune system cells, rendering adults and the elderly more vulnerable to infections than children and predisposing them to diseases associated with impaired immune system function.
An imbalance between beneficial and harmful bacteria may disrupt digestive system function, leading to chronic inflammation and affecting other systems, including the immune system.
Age-related dysbiosis can result from multiple factors, such as environmental toxins, food, and medications. These factors weaken the intestinal barrier cells, permitting pathogenic microbes in the gastrointestinal tract to infiltrate surrounding lymph nodes and stimulate the production of inflammatory substances. Consequently, the immune system’s normal cell production becomes disrupted.
Improper nutrition, whether excessive or insufficient, directly influences the immune system’s functionality. Impairment of the immune system during childhood can lead to chronic illness and hinder children’s growth.
As individuals age, their bodies require nutrients to maintain proper system function. Malnutrition, particularly protein-energy malnutrition, is linked to decreased immune system cells, cytokine release, and immune response to vaccinations.
Deficiencies in specific vitamins and minerals, such as zinc, selenium, and B6—common in the elderly—undermine their immune systems, making them more susceptible to infections than other age groups.


Chronic inflammation can directly impact the immune system’s function, ultimately impairing children’s physical and mental development.
Furthermore, it can heighten the risk and vulnerability to severe infections, including certain infections that healthy individuals with normal immune systems would not contract. A weakened immune system may impede the body from eliminating abnormally dividing cells, potentially leading to tumor development.
Pragmatic Approaches to Health Optimization
A burgeoning area of inquiry pertains to the interplay between gene disorders and immune system functionality, serving to elucidate the risk factors associated with disease development, particularly in the context of uncommon and rare diseases. In addition to the advancements in genetic engineering technology, the field of epigenetics holds promise by modulating gene expressions without manipulating the genes themselves. However, the nascent nature of this discipline necessitates further research prior to its application in clinical scenarios.

The consumption of prebiotics and probiotics contributes to the regulation of a beneficial gut microbiome equilibrium within the digestive system. Prebiotics, which are nondigestible polysaccharides or dietary fibers, stimulate the growth of gut bacteria, thereby cultivating a favorable environment for gut microbiome balance. Conversely, probiotics consist of live beneficial microorganisms that restore gut microbiota. Both prebiotics and probiotics contribute to the enhancement of gut microbiome health, stimulating the production of intestinal immune cells and exerting positive effects on the immune system as a whole.
The complexity of the immune system, with its myriad cells and chemical compounds, underscores the importance of obtaining a diverse range of nutrients to bolster its efficiency. Apart from the nutrients mentioned previously, other essential nutrients encompass proteins, the diverse amino acids of which underpin the production of crucial immune system components, water, and minerals such as potassium and chloride that perform pivotal roles in body temperature regulation.
Anti-free radical substances diminish chronic inflammation, shield body cells from cellular and chromosomal damage, and prevent cell degeneration and immune system dysfunction. Antioxidants, functioning akin to a battery, supply negative ions to free radicals and transport catalysts away from the cell in the ROS/RNS system, thereby curtailing oxidative stress chain reactions.
Antioxidants can be classified into enzymatic and non-enzymatic categories.
- Enzymatic antioxidants execute enzymatic functions, exemplified by Superoxide Dismutases (SODs), Catalase, and the Glutathione System.
- Non-enzymatic antioxidants encompass Ascorbic Acid (Vitamin C), Glutathione, Melatonin, Tocopherols and Tocotrienols (Vitamin E), Carotenoids, Flavonoids, and Uric acid.
Regular consumption of antioxidant-rich foods can aid in reducing the detrimental free radicals that potentially disrupt systemic and cellular DNA integrity.
Moreover, various natural extracts, including green tea, Resveratrol, Grape seed, Niacinamide (vitamin B3), and others, exhibit antioxidant properties.

As individuals age, the body experiences an inevitable deterioration, with numerous internal and external factors, both modifiable and immutable, contributing to the immune system’s decline across different life stages.
In response, Durascience™ has engineered the P.P.M™ (Pathogen Prevention Matrixes) component designed to foster robust immune system function, thereby safeguarding against infectious agents and averting the detrimental outcomes precipitated by pathogens. This approach prioritizes prevention over treatment, recognizing optimal health as the most precious asset and a resilient immune system as a foundational pillar of health. Therefore, it becomes vital to adopt preventative measures to fortify our bodies with a robust immune system.
